On Friday 4th November I gave a talk at Leadership and Quality of Care conference on Guernsey. Here is the text of the talk. Thanks to all for the great reception. And thank you for the invitation.
Introduction/preamble
Whether we are talking about healthcare in general, nursing in particular or certainly leadership there is always a strong tendency to focus on individuals: whether it’s the tale of the nurse who ‘really nurses from the heart’ and ‘always goes the extra mile’, or the heroic manager who has a vision of how things could be and single-handed brings everyone else on board. Or to look at the flip-side it could be the nurse who failed, who lost her caring nature, who lacked resilience, the bad apple in the batch as people were talking about a while ago. In this keynote I want to talk about the limits of leadership, and ask where all this talk of leadership came from. Then I want to argue that if you understand something of the political and policy context of much of today’s healthcare it can allow you to avoid taking on crushing personal responsibility for situations that have been brought about by others – by politicians and policy makers for example. This awareness can give you and your colleagues what I will call ‘critical resilience’.
The policy/political context for nursing work

In mainland UK the National Health Service has become, to put it colloquially, something of a plaything for governments on the right and left. A dangerous plaything, a booby-trapped football, if you like, that could explode at any moment. Set up within that wave of humanism that followed the second world war, it represents both a source of pride and a vulnerability. If it was ever assumed in the early days of the NHS that the service would abolish ill health and then could be closed down, the opposite has occurred. We see a growing range of expensive treatment options, and an ageing and more demanding population. Add to this the tendency of powerful professional monopolies to expand their services and encourage their use, alongside pharmaceutical companies looking for sales, then we have set of inbuilt problems that politicians of different political backgrounds have grappled with ever since.
Notable among this grappling, and I think the most important act, was the Thatcher Government’s attempt to turn the service into a ‘market’, the market, according to a neoliberalism which is still driving UK policy today, being the arrangement most likely to result in wealth—or efficiency in this case. The ‘internal market’ came and went but neoliberal governments’ distrust of unions and professional groups have flavoured their dealings with nurses, doctors and other healthcare professions ever since. They tend to see the professions as promoting their own interests and resisting change and I think there has to be some element of truth in that. But the last UK NHS reorganisation proposed by Andrew Lansley was opposed by virtually every professional group.
As well as controlling costs, all governments and their health ministers are keen to avoid the political embarrassment that trolley-waits or apparent care failures can lead to and to stamp their own signature on the service. This leads to constant reorganisations that—it is hard to deny—are wasteful of money, hugely wasteful of everybody’s time and provoke a high degree of anxiety because of constant threat and uncertainty. Couple this with public sector cuts, overt and covert, and a managerial demand to record more and more information, the work of nurses which is already difficult because of the nature of the work, can feel obstructed at every turn.
Reorganisations, turbulence and financial stringency
Governments hide the fact that so-called financial pressures on healthcare are in part at least, the result of decisions they have made, decisions about levels of taxation for example, or ideological beliefs about welfare and the role of the State. Sometimes the crises are presented as inevitable and impersonal, like the laws of physics. So talk of prioritising, rationalising and the apparent ‘need’ for efficiency become an accepted part of how States talk about welfare provision.
“The HSSD recognises that financial constraints brought about by changing tax legislation mean that real growth in funding is extremely limited. Additionally, there are significant additional pressures on finite resources due to the real inflation of health care interventions, the expectations of the public and patients, the existence of new and emerging treatments and interventions and the demography of Guernsey and Alderney. Given resource constraints, the HSSD cannot meet every healthcare need of every patient within its areas of responsibility. The HSSD therefore will need to make difficult choices between competing needs. The fact that the HSSD will need to take decisions not to commission specific services or interventions (even when they are cost-effective) is inevitable and therefore does not indicate that the HSSD is breaching its mandated obligations.”
(ETHICAL FRAMEWORK FOR PRIORITISING HEALTH CARE FOR THE STATES OF GUERNSEY Policy reference number: G1001 Version 2 Agreed by the HSSD on 24th April 2013)
New emphasis on care and compassion

But just when the pressures on health service organisations were at least consistent—focus on efficiency savings, reduce staff costs—we had the Staffordshire events – or rather the sudden publicising of the events and the government’s response to them and to the Francis Inquiry (I’m assuming that everyone here is familiar with that). So topics like the effect of the proportion of registered nurses on a shift and nurse to patient ratios started to be talked about along with, in my view, some less helpful ideas. I’ll leave it to you to decide whether ‘values-based recruitment’ and the six Cs are part of the solution or part of the problem. As I suggested earlier governments need above all to be seen to be doing something. Perhaps it is easier to give nurse recruits and those who recruit them extra hoops to jump through than to take the idea seriously that toxic work environments – and some of that toxicity is of governments’ own making – can eventually corrupt the most apparently “high-scoring” compassionate nurses.
Leadership is the key – of successes and failures
Look at a report into any recent healthcare scandal and you are likely to find at least part of the blame put on ‘lack of leadership’.
“As a result of poor leadership and staffing policies, a completely inadequate standard of nursing was offered on some wards in Stafford. The complaints … testified not only to inadequate staffing levels, but poor leadership, recruitment and training. This led in turn to a declining professionalism and a tolerance of poor standards… (page 45) It is a truism that organisational culture is informed by the nature of its leadership… (page 64) The common culture and values of the NHS must be applied at all levels of the organisation, but of particular importance is the example set by leaders.” (page 78) (Francis 2013)
‘Leadership’ for the last 35 years has been seen as the solution to problems and challenges from international economic competitiveness to the need to motivate staff in a hospital ward. [trump slide] But much of this faith in leadership is based on assumptions and myths, fuelled by a multi-billion dollar industry involving leadership and management institutes, training courses and best-selling paperback publications, as well as media promotions of stereotypes of business managers. Of course ideas about leadership and good management do have usefulness—once we get past the exaggerated expectations and the poorly thought through assumptions. Groups of people can work together either relatively well or extremely poorly and some of this is down to how those in charge conduct themselves. [Recent reports about patient safety by Don Berwick (Berwick 2013) and poorly performing NHS trusts and Bruce Keogh (Keogh 2013) give some practical guidance about effective leadership. The work of organisational psychologists also reveals the usefulness of good approaches to leadership (West 2014).]
Today’s discussion of management and leadership can be traced to the beginning of business schools in the US and Europe and they developed in response to the rise of industrial production and the increasing complexity of civil administration. The first business school in the UK was created in 1902 in Birmingham.
As well as business schools, we have seen a growth in popular books, organisations and Internet sites promoting particular ideas about business success, often closely identified with a charismatic and successful individual. The 1980s saw the landmark book In Search of Excellence: Lessons from America’s Best-Run Companies by Peters and Waterman. Tom Peters’ website describes him as ‘almost single-handedly “inventing” the public “management guru industry,” now global in scope and billions of dollars in size’ (http://tompeters.com/about/toms-bio/ ). Note the strong element of individual heroism, its an almost essential feature of these popular presentations of leadership. Even though the leader in question may be presenting a more nuanced version of leadership it is their own successes that are drawn on to give them the authority to tell others how to do it. So despite evidence to the contrary and more up to date ideas in organisational studies, leadership is still strongly influenced by individualistic ideas.
There are countless lists of so-called styles of leadership: transactional and transformative leadership, charismatic leadership and often these are highly idealized pictures.
With a nursing audience it is important to knowledge that the story of leadership is so often the story of men.

‘the characteristics people typically associate with leadership are often stereotypically masculine.. – conventionally masculine descriptors such as “assertive,” “forceful,” “dominant,” and “competitive.” …The alignment of the stereotypical characteristics of men and the stereotypical characteristics of good leaders makes it easier for men to be perceived as successful leaders… (Eagly and Koenig 2014)
Leadership in healthcare
Leadership in today’s sense was first promoted in the UK health service in the mid 1980s, during the period of Margaret Thatcher’s government. Traditionally, right wing governments in the UK have been more impatient with the welfare sector than their left wing opponents because the Welfare State is generally seen as a creation of the left.
One contemporary critique of the NHS has been that the service as a whole has become like a vast and slow machine with no one taking responsibility for guiding its overall direction or for promoting change and improvement. In the market vocabulary of the 1980s to the present day, the health service showed little responsiveness to its customers and operated for its own convenience rather than that of those who use or rely on the service.
The 1990s saw the rise of managerialism, the attempt to introduce management approaches and practices from the business world into the public sector—particularly healthcare. Governments confronted the major professions and their key weapon was to put in place increasingly coercive management structures along with systems for measuring ‘performance’ and with ‘naming and shaming’ organisations or even individuals who appeared to depart too far from norms or fail to meet targets. However, the disadvantages of this approach have emerged recently with key reports into NHS problems tending to highlight the need for more collaborative forms of leadership where mistakes can be learnt from in a so called no-blame culture (Berwick 2013; West 2014).
What does a nursing leader look like? –
Here are some possible answers, features that might differentiate the nursing leader from the organisational manager – though of course many are (trying to be) both:
Nursing leaders can, and do, articulate what nursing, and being a nurse, is about
They understand and share your professional aspirations and frustrations
Something about them—their behaviour and achievement—makes them role models
They argue the case for nursing resources and influence within organisations and in public
They are confident enough in their commitment to nursing to sometimes criticise it, if necessary, in public
Many consider that good leadership at ward and clinic level is essential to maintain standards of patient care. It is probably not difficult to list, as above, desirable qualities and behaviours of these leaders. Nursing magazines are full of such lists and urgings to nurses to be better at them. However, professional leadership happens in a context and in certain contexts it becomes limited and even blocked by managerialism or powerful other professions. Now some of you might find my focus on limitations depressing. But my point is that if individual nurses are continually exhorted to perform better as a leader or as a nurse and the structural obstructions and difficulties they face are glossed over then it is likely that those individuals eventually blame any lack of impact on their own failure to try hard enough.
The need for critical resilience

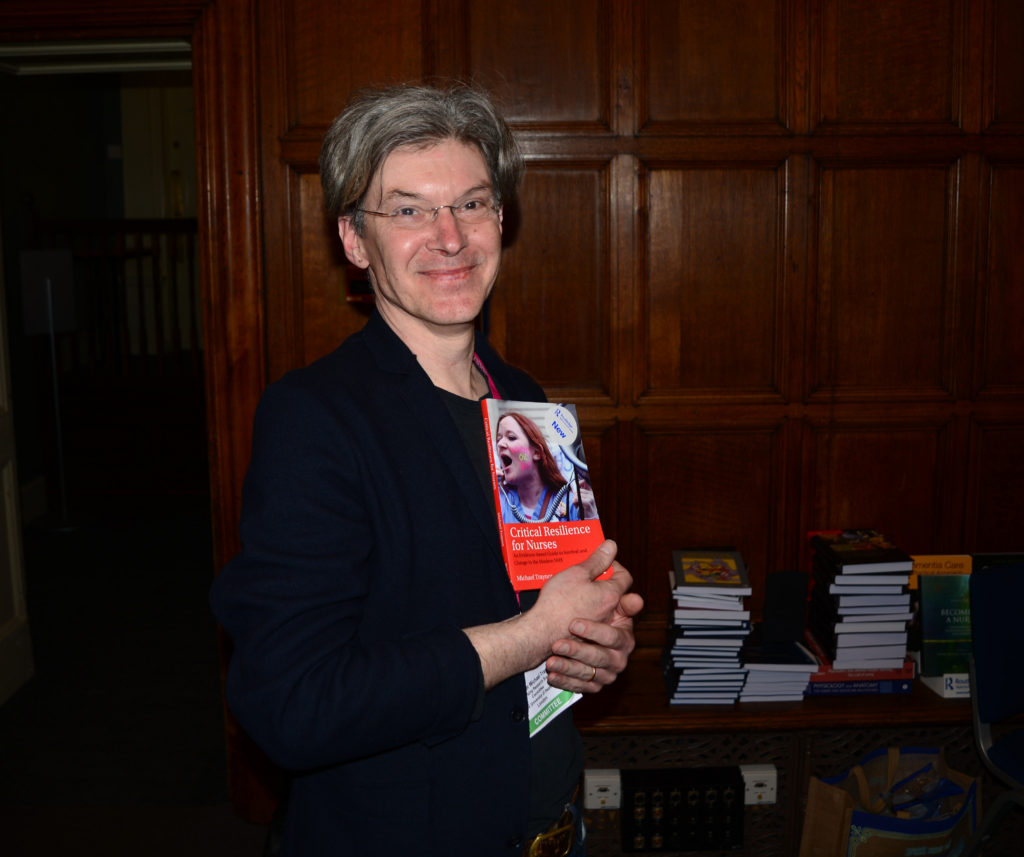
I have just written a book called Critical Resilience for Nurses – its out in March. In it I try to point out some of the unhelpful aspects of a current promotion of this idea of ‘resilience’ – among nurses but also more widely. Resilience is often pictured in nursing writing as a kind of skill, like aseptic technique, that nurses can be taught so that they can last a little longer before burning out. But research into resilience was a response among psychologists to the puzzle that some children seemed to apparently survive adverse childhoods better than others. Most child psychologists realised that this ‘resilience’ was generated by something in the environment just as much as personal characteristics. So my book is a call for nurses to get together, to form critical discussion groups, and I spend some pages spelling out the difference between complaint and critique, and to understand the structural forces that thwart their intentions to nurse to a high standard. I mentioned some of these earlier.
I want to end by talking about the Radical Nurses Group founded in the 1980s. The group ‘refused to cope’. They made a badge with this slogan. They meant, I think, that nursing did not do itself—or healthcare—any favours by grudgingly putting up with a series of cuts and indignities, complaining but never taking action. The slogan on their badge reminded me of a piece in a book about photography, written by critic John Berger, looking at an image of the dead Cuban revolutionary Che Guevara taken in 1967.

Guevara was well aware that his stance and his actions might well lead to his death and he put in writing the fact that he had no reservations about this. He fought, to put it very simply, against injustice and exploitation and knew how strong their forces were. Berger writes: ‘His envisaged death offered him the measure of how intolerable his life would be if he accepted the intolerable condition of the world as it is.’ (Berger 2013 p. 8). This word ‘intolerable’ is repeated throughout the chapter on Che. Later Berger writes, ‘The world is not intolerable until the possibility of transforming it exists but is denied’. In contrast to the world’s poor, nurses in the UK are privileged. However as people who deal, on a daily basis sometimes, with extremes of suffering and death, it seems not far-fetched to sometimes see the conditions that others expect them to do this work in as exploitative, exploitative of their urge to help others for example. I cannot help but see the suggestion that nurses cope better and learn how to be more resilient as, wittingly or not, a part of that exploitation. That is why that small badge offers so much power. What is intolerable should be named as such not put up with.
Summing up
In talks like this all over the UK, speakers try to inspire nurses to do better and try harder – to be more caring, more articulate, more assertive, more evidence-based, to be better leaders. The nursing press is full of it and full of examples of nurses who have achieved genuinely amazing things. That’s great. That’s at one end of the spectrum if you like. Then, at the other end of public nursing talk is complaint: ‘I care for others but no body is caring for me – not governments or managers or nursing bodies’. But I think it is an often un-thought-through stance. What we don’t get enough of in popular nursing discourse is intelligent critique: what are the components of this apparent neglect of nursing, how did they arise, from which groups, what problems are they trying to solve, what might their guiding intentions be? Without this critique we easily fall back on individual blame: a failure of leadership, a lack of resilience, a lack of compassion. So this talk is a very short attempt to address a few of those questions. But it is much better done in groups – like the Radical Nurses Group I mentioned just now. This talk is a call for nurses to get together and to get informed.